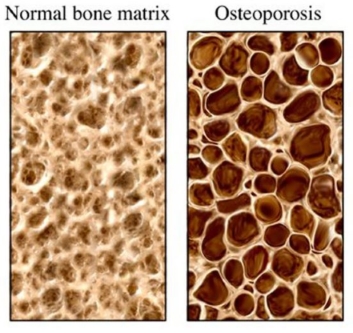
Osteoporosis is the bone condition characterised by low bone mass, which is associated with with reduced bone strength and an increased risk of fractures. Osteoporosis occurs most commonly in postmenopausal women. Low bone mass may be related to either inadequate peak bone mass acquisition and/or ongoing bone loss.
Risk factors for osteoporosis (causing bone loss):
- Overactive thyroid (hyperthyroidism)
- Advanced age
- Previous fracture
- Long term glucocorticoid therapy
- Low body weight (less than 58kg)
- Family history of hip fracture
- Cigarette smoking
- Excessive alcohol intake
- Drop in estrogen (late onset of menstrual periods, absent or infrequent periods and premature early menopause before age of 45)
- Pituitary gland failure (hypopituitarism)
- Chronic illness such as chronic liver disease, chronic kidney disease, coeliac disease, rheumatoid arthritis, systemic lupus erythematosus
- Lack of physical activity
- Low Vit D
- Low Calcium intake
- Eating disorders such as anorexia nervosa and bulimia
Patients with osteoporosis has no specific pain or symptoms. However, it does increase the risk of fractures if the patient has a minor fall. Common fractures associated with osteoporosis are Colles's fracture (fracture of wrist) and hip fracture.
Fracture risk assessment tool can be used to estimate the 10 year probability of hip fracture or major osteoporotic fractures combined (hip, spine, shoulder or wrist) for untreated patient with or without information on DXA scan.
Currently, the most reliable way to diagnose osteoporosis is to measure bone density using DXA scan. DXA scan works similar like normal x-ray and has a low radiation dose. Bones of lower back (lumbar spine) and hip region (proximal femur) are measured. In special cases the bone in forearm (radius) may be measured.
Patient can qualify for a Medicare rebate for a DXA scan if:
- Aged 70 years and over
- One or more fractures occuring after minimal trauma
- Monitoring of low bone mineral density proven by previous DXA
- Prolonged steroid therapy
- Female oestrogen deficiency (hypogonadism) lasting more than 6 months before age of 40
- Primary hyperparathyroidism (high parathyroid hormone)
- Chronic illness such as chronic liver disease, chronic kidney disease, coeliac disease, rheumatoid arthritis, systemic lupus erythematosus
- Overactive thyroid (hyperthyroidism)
Management of osteporosis:
- Calcium intake. Adults who have adequate dietary and supplements intake of calcium 1000 mg/day do not need to take calcium supplements. Women older than 50 year old and men older than 70 year old should have dietary and supplements intake of calcium of 1300 mg/day. NB: Research did not show that taking calcium supplement can increase cardiovascular risk.
- Vitamin D. Men and women should have 800 IU of Vitamin D daily. Higher doses are required if they have malabsorption or rapid metabolism of Vit D due to use of anticonvulsant medication.
- Exercise. Women with osteoporosis (or who want to prevent it) should exercise for at least 30 minutes three times per week.
- Stop smoking
- Limited alcohol and caffiene intake
- Oral bisphosphonates. Recommended as first line therapy for men and postmenopausal women with osteoporosis due to efficacy, favourable cost and the availability of long term safety data. Alendronate or Risedronate are preferable. Oral bisphosphates should be avoided in patient with esophageal disorders, medication compliance or chronic kidney disease (eGFR <30mL/min). This medication will need to be taken weekly or monthly depending on the regimen of the treatment.
- Intravenous bisphosphonate. Intravenous infusion of Zoledronic acid once yearly can be offered to patients who can take oral bisphosphonates. This can be organised by a doctor through Lifescreen Australia.
- Denosumab is a humanised monoclonal antibody against RANKL (receptor activator of nuclear factor kappa-B ligand) that reduces osteoclastgenesis. It can be used as alternative or initial therapy for patients with high risk fracture, such as older patients with difficulty with dosing requirements of oral bisphosphonates or poor renal function. It is administered through subcutaneous injection every 6 months.
- Parathyroid hormone. Teriparatide can be used in men or postmenopausal women with severe osteporosis. This drug should be used for short term and can only be prescribed by specialist. Criteria for PBS can be found here.
- Selective estrogen receptor modulators. Raloxifene can sometimes be used in postmenopausal women. It has beneficial effect of reducing breast cancer risk but increase deep venous trombosis and hot flushes.
- Testosterone replacement therapy can be used in hypogonadal men (clinical symptoms and signs consistent with androgen deficiency and a distinctly subnormal serum testosterone concentration) or men who have an unequivocal cause for hypogonadism (eg. pituitary tumour, Klinefelter syndrome, GnRH deficiency) and who do not have contraindications to testosterone therapy. NB: Due to abuse by some prescribing GPs, restriction had been enforced on this. For more information, please click here.
- Estrogen therapy. In premenopausal women with amenorrhoea from various causes, treatment should be directed at underlying cause. If resumption of menses is unlikely, estrogen therapy is usually the treatment of choice. Oral contraceptive pill usually indicated in this situation. A lack of period is usually associated with low estrogen levels, which reduces bone density.