Introduction
• Variably sized papules or nodules.
• Cysts can be divided into true cysts with an epithelial lining (histologically and sometimes visible clinically) and false cysts without such a lining.
• Appreciation of the actual size of the cyst often requires palpation.
• Different types of cysts often have characteristic anatomic locations and histologicfeatures.
• Treatment of true cysts (if symptomatic) is primarily surgical.
True Cysts – Common
Epidermoid Inclusion Cyst (EIC) (Epidermal Inclusion Cyst, ‘Sebaceous Cyst’)
• Most commonly on the face and the trunk; skin-colored to yellow-white unless inflamed; size varies from several millimeters to centimeters.
• A visible comedonal-like opening or pore (resembles a blackhead) may be seen on the surface of the papule or nodule (Fig. 90.1A).
• A soft cheese-like, sometimes malodorous, material composed primarily of keratin can usually be expressed from the opening.
• Cyst contents may rupture into the dermis, eliciting an acute and chronic inflammatory reaction, leading to significant redness and pain; this inflammation is often confused with a bacterial infection (Fig. 90.1B).
• Most commonly sporadic; multiple lesions rarely associated with Gardner syndrome or Gorlin syndrome.
• DDx: see Fig. 95.17.
• Rx: inflamed lesions: if fluctuant, can be incised and drained ± packed with gauze (a wick); if nonfluctuant, can be injected with intralesional CS; non-inflamed (‘cold’) lesions can be excised surgically but may result in a significant scar.
Milium (Milia – Plural)
• A small, superficial (1–2 mm), firm cyst that is white in color and is sometimes confused with a whitehead (Fig. 90.2); occasionally they are grouped.
• Occurs most frequently on the face, especially the periorbital region; seen in both children and adults.
• Commonly observed on the face in newborns; in this setting, they often resolve spontaneously.
• The majority of patients with multiple facial milia have no underlying condition; however, there may be a secondary cause (Table 90.1).
• DDx: whitehead (closed comedone), syringoma.
• Rx: because a milium lies beneath intact epidermis, the lesion must be punctured with a needle or sharp blade in order to express the keratin contents.
Pilar Cyst (Wen)
• Most common location is the scalp; sometimes there is associated overlying alopecia (Fig. 90.3).
• Solitary or multiple relatively firm nodules.
• May be inherited (autosomal dominant).
• Surgical removal is easier than for an EIC because less dissection from surrounding normal tissue is required; a small incision with lateral pressure may be all that is necessary.
Pilonidal Cyst
• Most common location is the upper gluteal cleft in association with a sinus tract ± fragments of hairs.
• May have a history of draining malodorous material.
• More common in men.
• May be associated with acne conglobata, hidradenitis suppurativa, and dissecting cellulitis (follicular occlusion tetrad).
True Cysts – Less Common
Vellus Hair Cyst
• 2- to 3-mm, skin-colored to brown-blue papule(s), commonly on the trunk (Fig. 90.4).
• Occasionally inflamed.
– When multiple, may be inherited (autosomal dominant); can be associated with pachyonychia congenita 6b/17 > 6a/16.
– Bedside diagnostic test: nick the cyst and examine expressed contents for vellus hairs.
• DDx: acne, steatocystomas (can be overlap).
Steatocystoma
• 2- to 10-mm, skin-colored to pigmented papule or nodule, usually multiple and grouped; commonly develop on the trunk or in the axillae and groin (Fig. 90.5).
• May drain oily fluid.
• Multiple lesions may be inherited as an isolated finding (autosomal dominant, KRT17 mutation) or represent a clinical feature of pachyonychia congenita 6b/17 > 6a/16.
Hidrocystoma
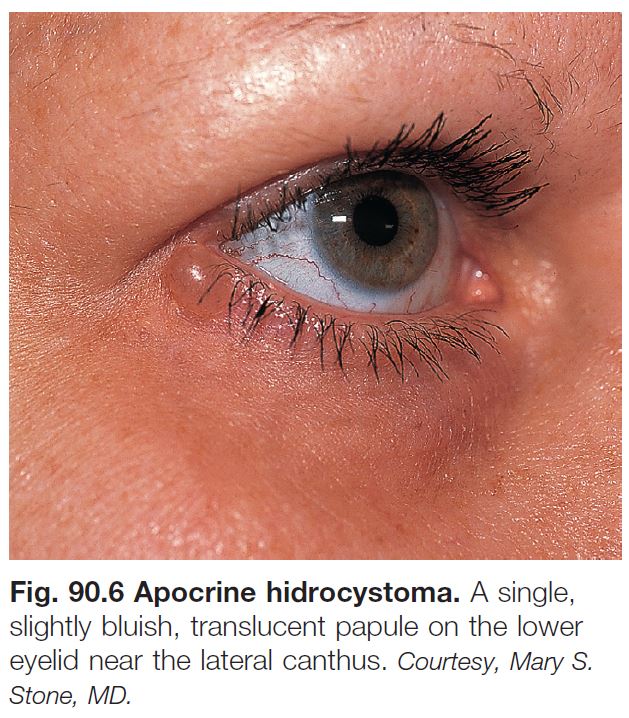
APOCRINE
• Often a solitary, translucent to bluish papule on the eyelid margin (Fig. 90.6).
• Histology: the lining resembles that of an apocrine gland (decapitation secretion).
• Rx: if bothersome or symptomatic, excision by an experienced surgeon.
ECCRINE
• Multiple or solitary bluish, translucent papule(s) on the face (Fig. 90.7).
• Can become more prominent with sweating.
• Bedside diagnostic test: nicking the surface results in drainage of clear liquid.
‘False’ Cysts (No True Epithelial Lining)
Mucocele
• Compressible mucosal-colored to bluish papule or nodule, most commonly seen on the lower, inner mucosal lip (Fig. 90.8).
• Secondary to disruption of the minor salivary ducts.
• May resolve spontaneously.
• Rx: if persistent, excision or other destructive procedure, intralesional CS.
Digital Mucous Cyst
• Translucent, skin-colored to bluish papule or nodule most commonly on digits, in particular the dorsal, distal finger near the distal interphalangeal joint (Fig. 90.9).
• There may be a connection to the joint space.
• Occurs in the setting of osteoarthritis.
• Longitudinal nail deformity may be present when the lesion compresses the nail matrix.
• Puncture can result in drainage of a gelatinous material.
• Rx: observation, intralesional CS, repeated incision and drainage, excision.
Ganglion Cyst
• Soft, cystic nodule most commonly on the wrist > ankle.
• Seen more often in women than in men.
• Rx: may spontaneously resolve but recurrence common; treatment modalities include compression, aspiration and intralesional CS, excision.
Pseudocyst of the Auricle
• Painless swelling, generally unilateral, of the scaphoid fossa of the ear (Fig. 90.10).
• More common in men than in women.
• Rx: aspiration ± intralesional CS, incision and drainage; any treatment should be followed by pressure dressings.










 Preauth
Preauth