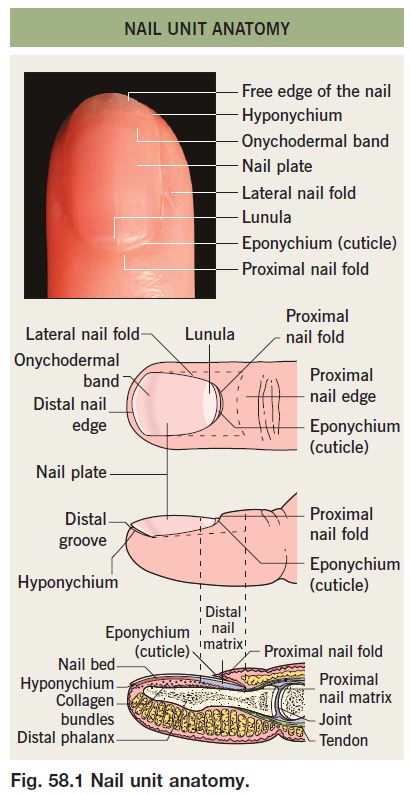
• The nail matrix, which is the growth area, has proximal and distal components (Fig. 58.1).
– The proximal nail matrix forms the top (surface) of the nail plate.
– The distal nail matrix forms the underside of the nail plate; therefore, biopsies of the distal matrix are less likely to produce a deformity of the surface of the nail plate.
• Fingernails grow ~1 mm per month and are replaced every 6 months.
• Toenails grow ~0.5 mm per month and are replaced every 12 months.
• Therefore, nail plate abnormalities such as Beau’s lines that are due to insults to the nail matrix can be dated by their distance from the cuticle.
• Rx of common nail disorders is given in Table 58.1.
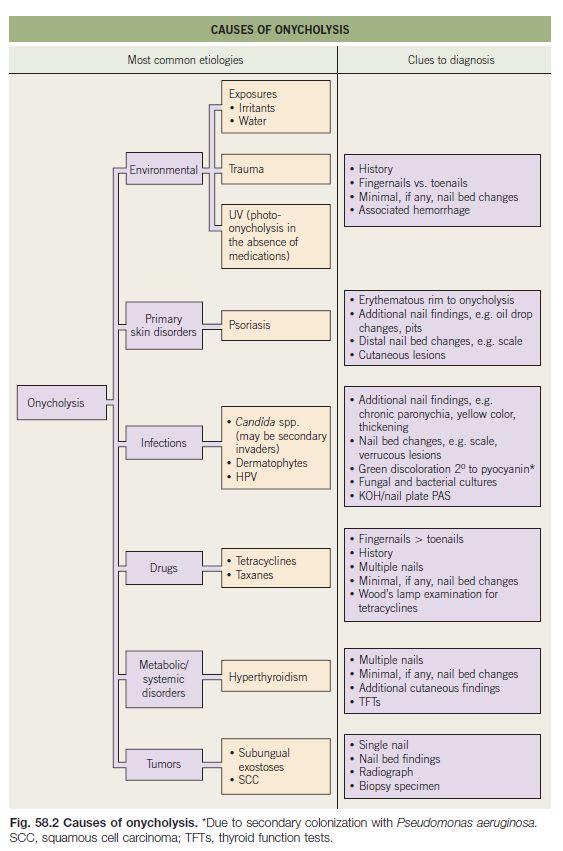
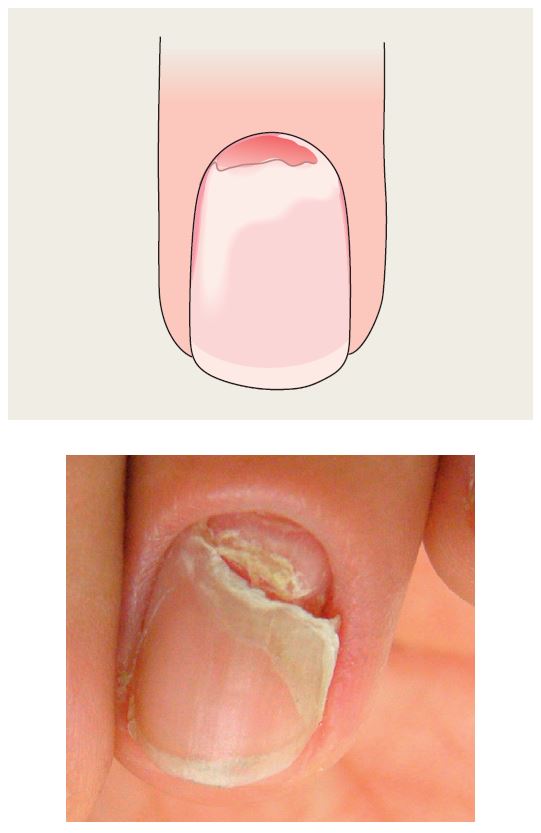
Onycholysis
• Distal nail plate detachment, causing nail to look white to yellow-white (Fig. 58.2).
• Chronic exposure to water and irritants (e.g. soaps) is a common cause.
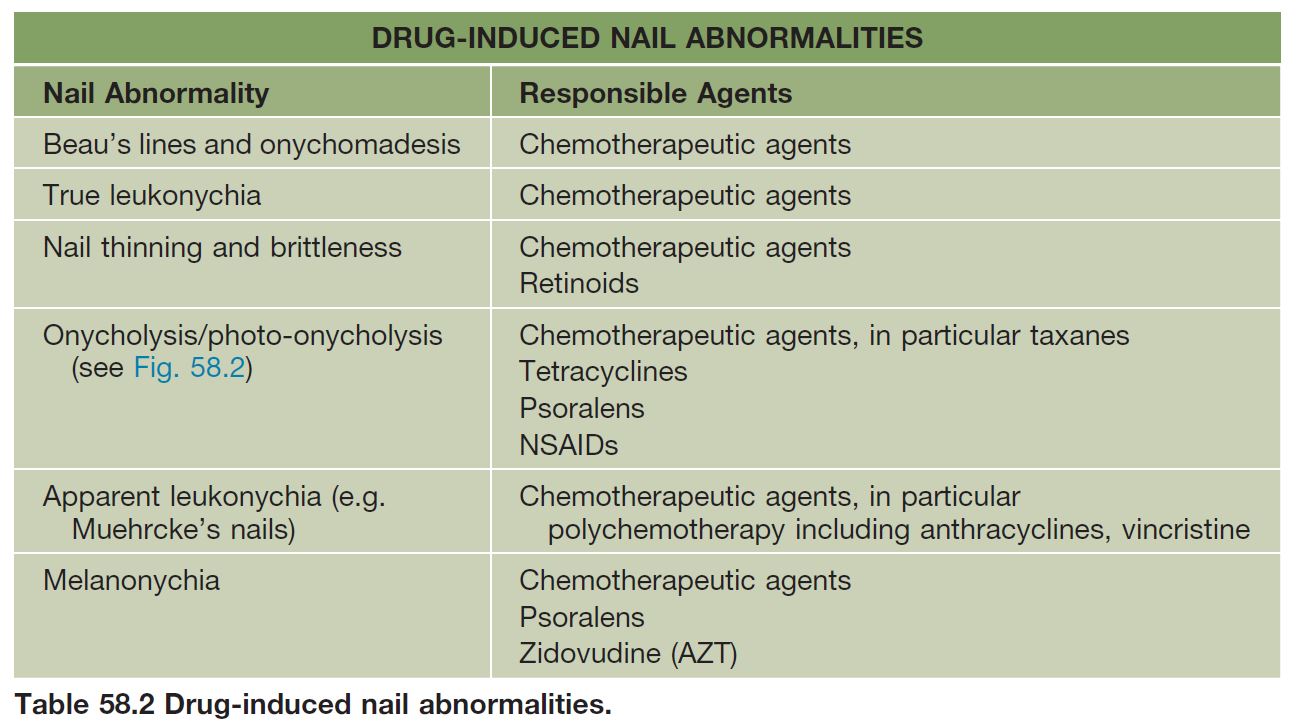
• Associated with psoriasis, onychomycosis, hyperthyroidism, and medications (Table 58.2).
Onychomadesis
• Proximal detachment of nail plate.
• When single digit, often due to trauma.
• Consider systemic cause (e.g. high fever, chemotherapy, post-erythroderma, post-viral) if multiple nails involved.
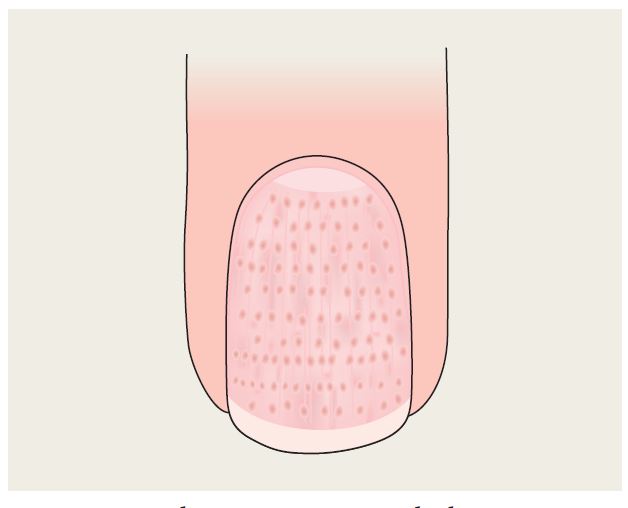
Pitting in Psoriasis
• Punctate depressions in the nail plate.
• Admixed with oil drop changes and other signs of nail psoriasis such as onycholysis, subungual debris (see Chapter 6).
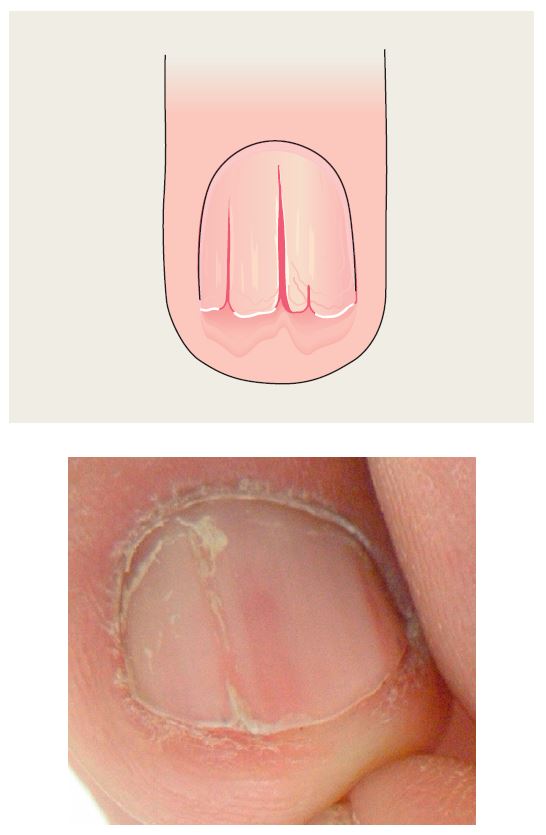
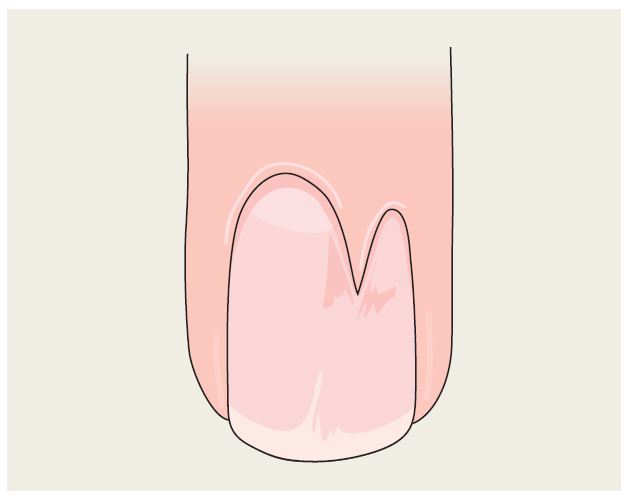
Darier Disease
• Alternating longitudinal red and white streaks (i.e. erythronychia and leukonychia).
• Distal fissuring (notches).
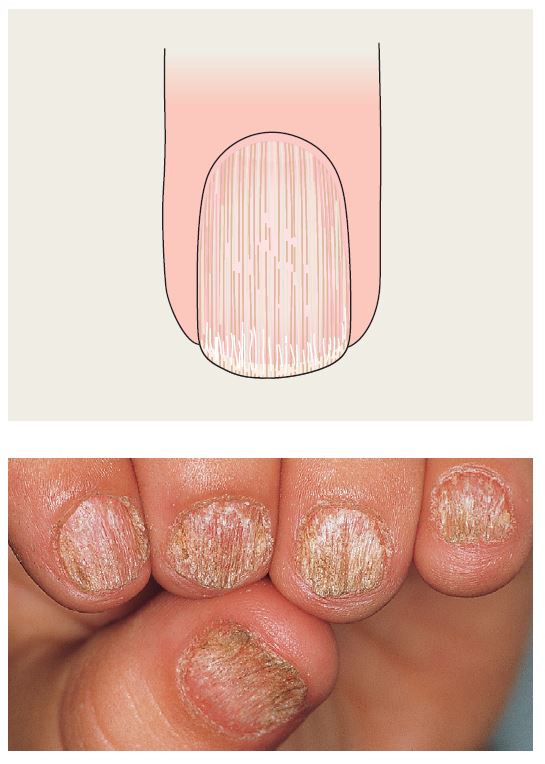
Trachyonychia
• Rough, ‘sandpaper’ nails, often thin.
• Associated with alopecia areata or lichen planus >> psoriasis.
• May affect most or all nails, especially in children; often termed ‘20-nail dystrophy’.
Lichen Planus
• Nail thinning/atrophy, especially laterally.
• Sometimes dorsal pterygium (see below).
• See Chapter 9.
True Leukonychia
• White discoloration of nail.
• Punctate most common.
• Punctate > linear > diffuse.
• Linear bands may be transverse or longitudinal (see Darier disease).
• Punctate or transverse linear forms often due to trauma.
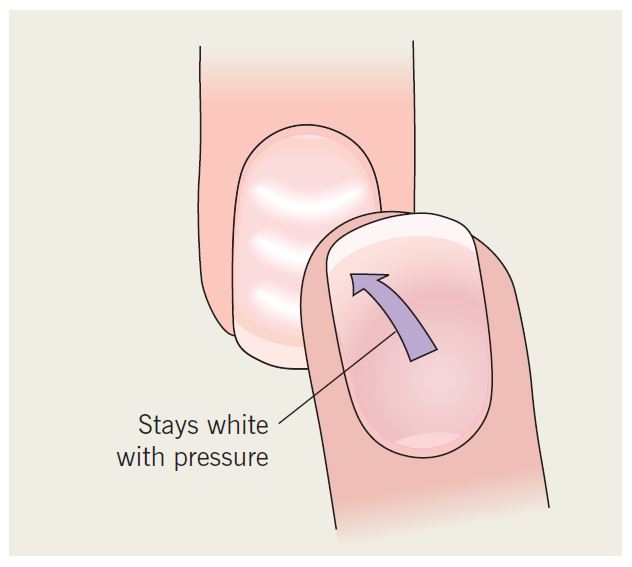
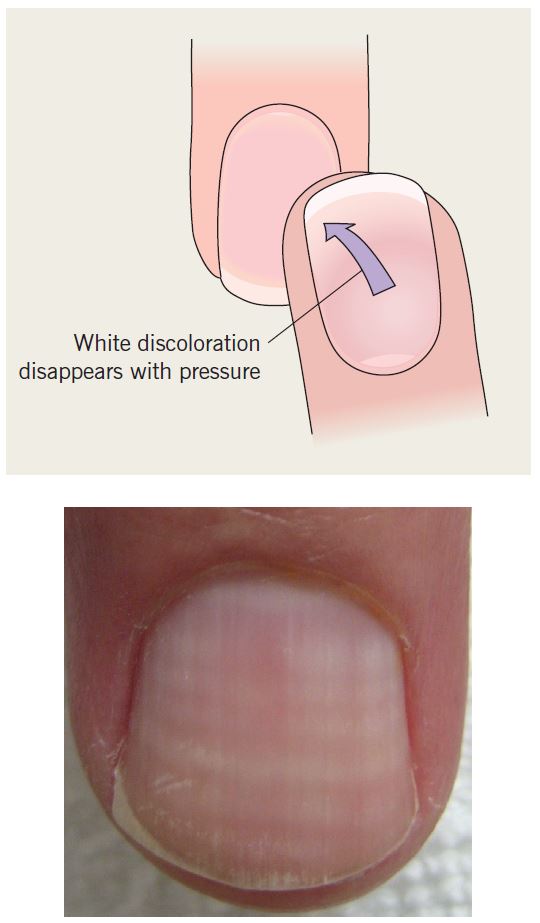
Apparent Leukonychia
• Nail plate appears white due to alterations in nail bed (e.g. edema).
• Secondary to drugs or systemic disease (e.g. hypoalbuminemia leads to Muehrcke’s lines).
• Terry’s nails: only distal several millimeters of nail plate unaffected; associated with liver disease.
• Lindsay’s nails: proximal half of nail is white and distal nail is red; associated with renal disease.
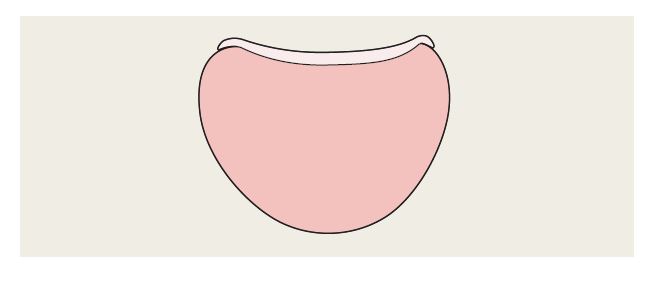
Koilonychia
• Spoon-shaped nails.
• Physiologic in children, associated with iron deficiency in adults.
• Transverse depressions in the nail plate.
• Often secondary to trauma.
• Consider systemic insult (e.g. high fever, chemotherapy) if multiple nails involved.
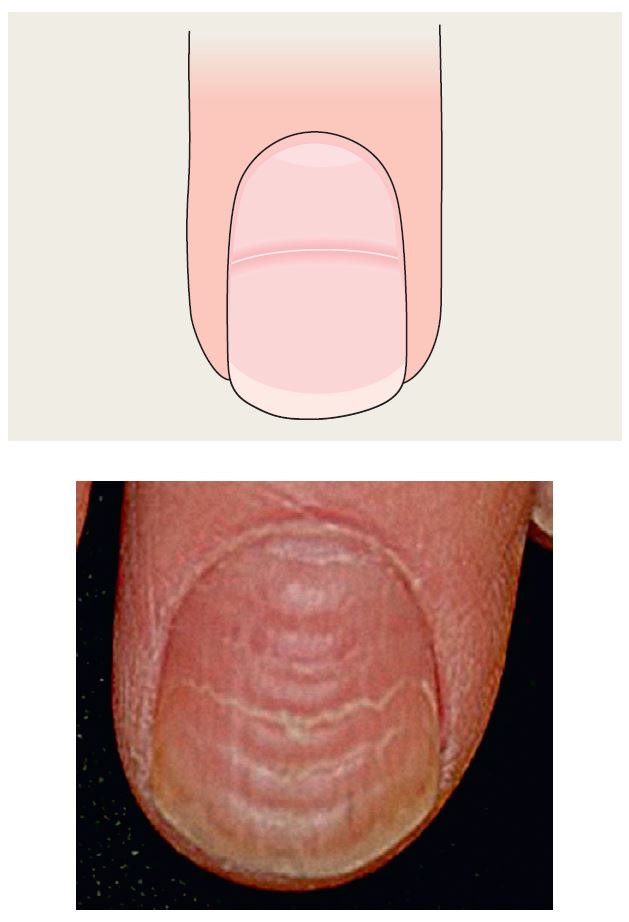
Beau’s Lines
• Transverse depressions in the nail plate.
• Often secondary to trauma.
• Consider systemic insult (e.g. high fever, chemotherapy) if multiple nails involved.
Longitudinal Melanonychia
• Longitudinal brown-to-black band.
• Multiple bands common in darker skin types (physiologic); also can be due to trauma (Table 58.3).
• Single band may be a sign of nail melanoma (Table 58.4).
• When melanoma is suspected, the nail matrix must be biopsied (see Fig. 58.1).
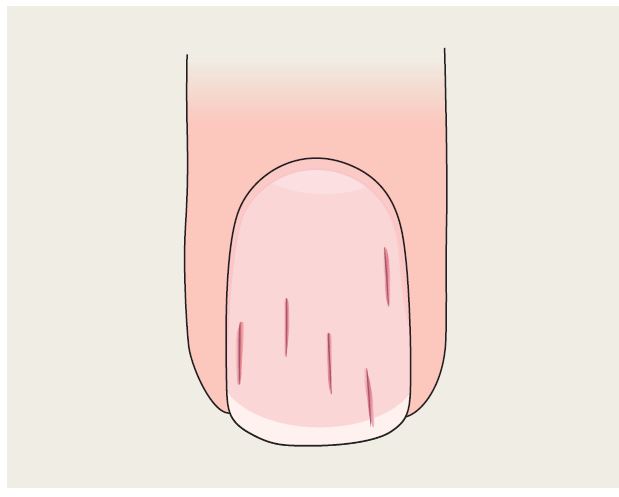
Onychorrhexis
• Thinning and longitudinal ridging.
• May develop fissuring or notching.
• Less pronounced than trachyonychia.
• Normal finding with aging.
• Sometimes secondary to trauma.
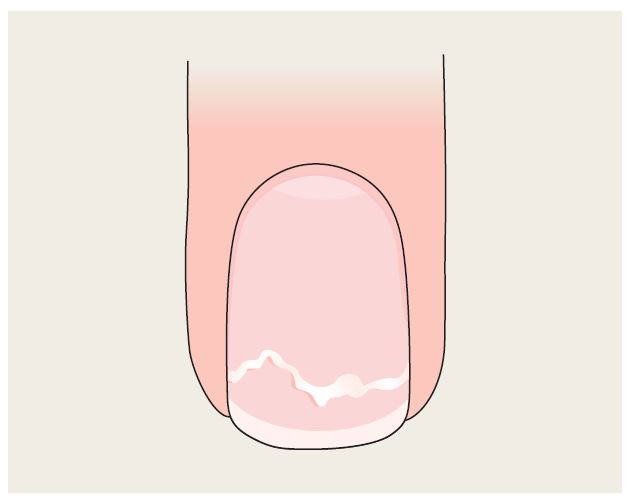
Onychoschizia
• Lamellar splitting of distal nail into multiple layers.
• Associated with the use of soap and irritants.
• Normal finding with aging.
Pitting in Alopecia Areata
• Punctate depressions in nail plate; geometric or ‘scotch-plaid’ pattern.
• Compared to psoriasis, pits are smaller and more numerous.
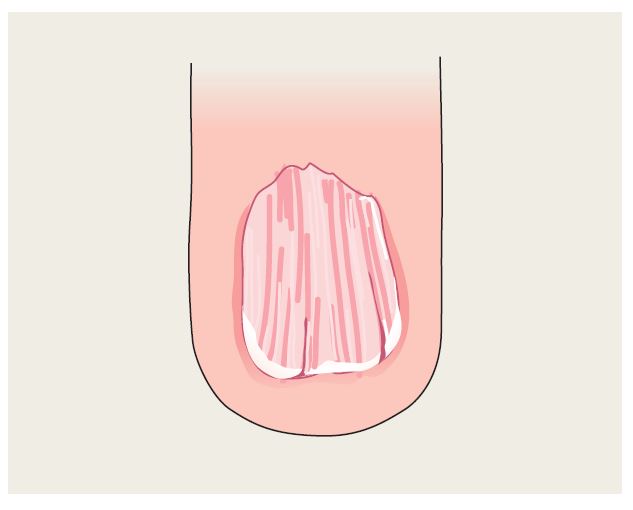
Dorsal Pterygium
• Triangular extension of the proximal nail fold into the nail bed.
• Local loss of nail plate.
• Associated with lichen planus.
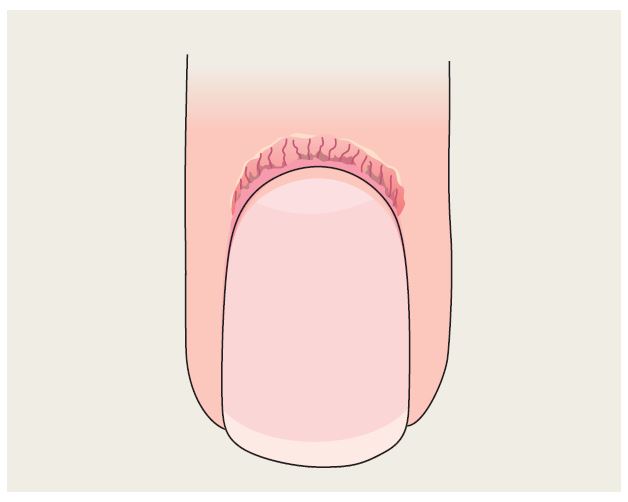
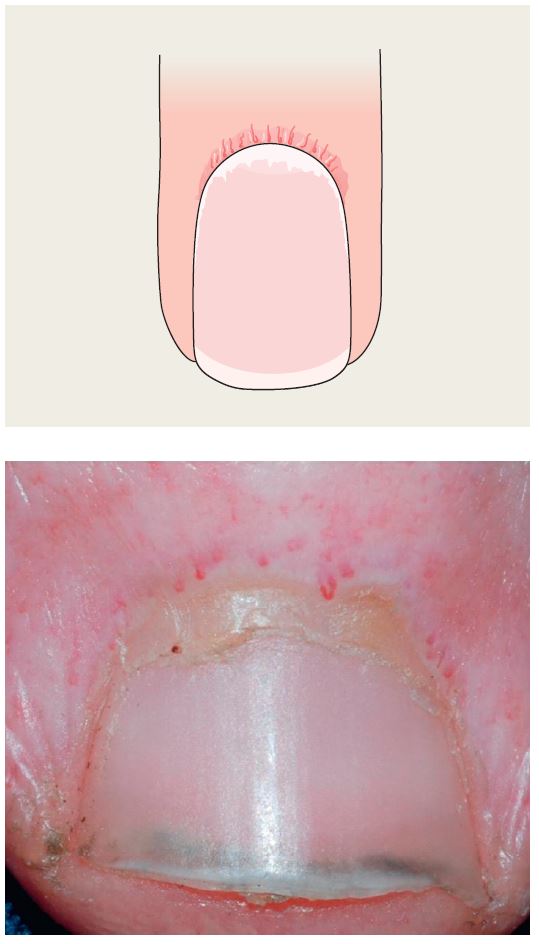
Proximal Nail Fold Telangiectasias
• Capillary prominence ± cuticular hemorrhages.
• Associated with lupus erythematosus and Osler–Weber–Rendu syndrome.
• Also associated with dermatomyositis and scleroderma, with a slightly different appearance (see below).
Proximal Nail Fold Telangiectasias with Capillary Dropout
• Capillary dropout alternating with dilated capillary loops.
• Associated with dermatomyositis and scleroderma.
• In dermatomyositis, ragged cuticles may also be present.
• In scleroderma, ventral pterygium (loss of distal subungual space) may be seen.
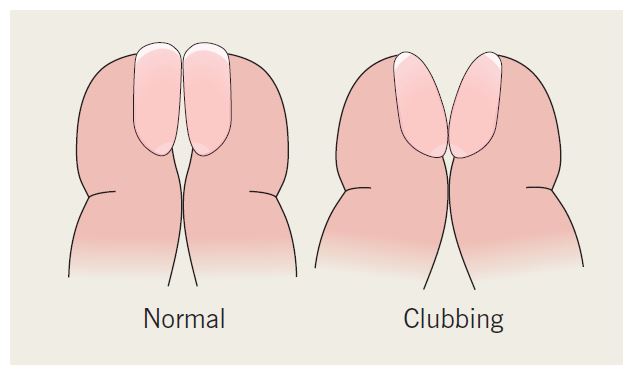
Clubbing
• Bulbous digits with watch-glass nails (> 180° angle between proximal nail fold and nail).
• Most commonly seen in thyroid acropachy and in association with cardiovascular and bronchopulmonary disorders.
Splinter Hemorrhages
• Thin, longitudinal, dark-red subungual lines.
• Usually secondary to trauma.
• Can be seen in psoriasis, endocarditis.
• Pattern due to topography of nail bed.
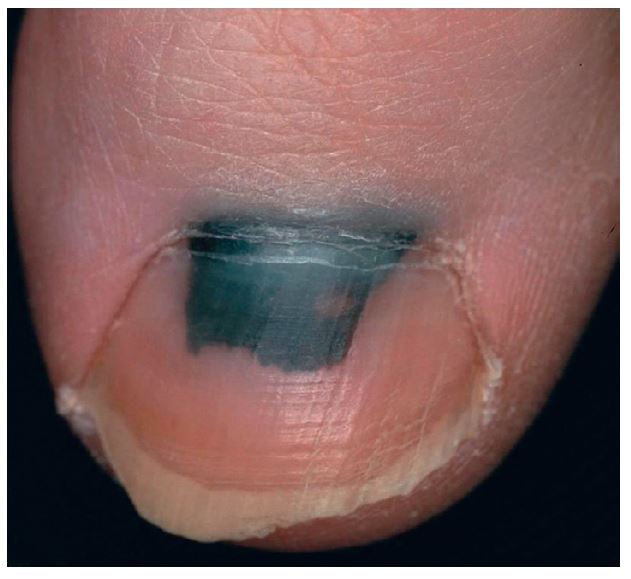
Subungual Hematoma
• Purple-red to black color beneath nail plate.
• Moves distally with nail growth.
• Secondary to trauma; if cuticle pushed back, band of normal nail growth may be seen.
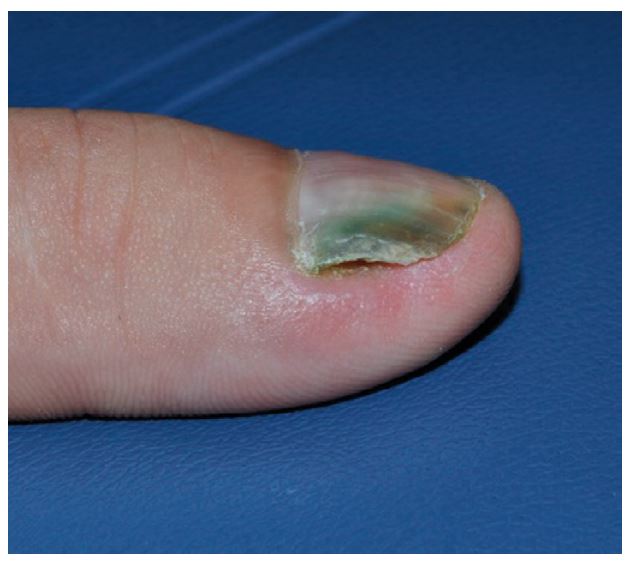
Green Nail
• Blue-green to green-black discoloration secondary to Pseudomonas aeruginosa.
• Usually in association with onycholysis (creates a favorable moist environment).
Paronychia, Acute
• Swollen nail fold with erythema and pain, sometimes with pustular drainage.
• Caused by bacteria (especially staphylococci).
• Recurrent episodes may be caused by herpes simplex virus infection (herpetic whitlow).
Paronychia, Chronic
• Chronic proximal nail fold inflammation with loss of cuticle (natural sealant).
• Exacerbated by exposure to water and irritants or overaggressive nail grooming.
• May have secondary Candida colonization.
Pustular Psoriasis
• Pustules can form under the nail.
• May have lesions of psoriasis on the tips of the digits.
Median Nail Dystrophy (Tic Deformity)
• Thumbnail(s).
• Multiple transverse grooves with central longitudinal depression.
• Due to manipulation of skin overlying matrix
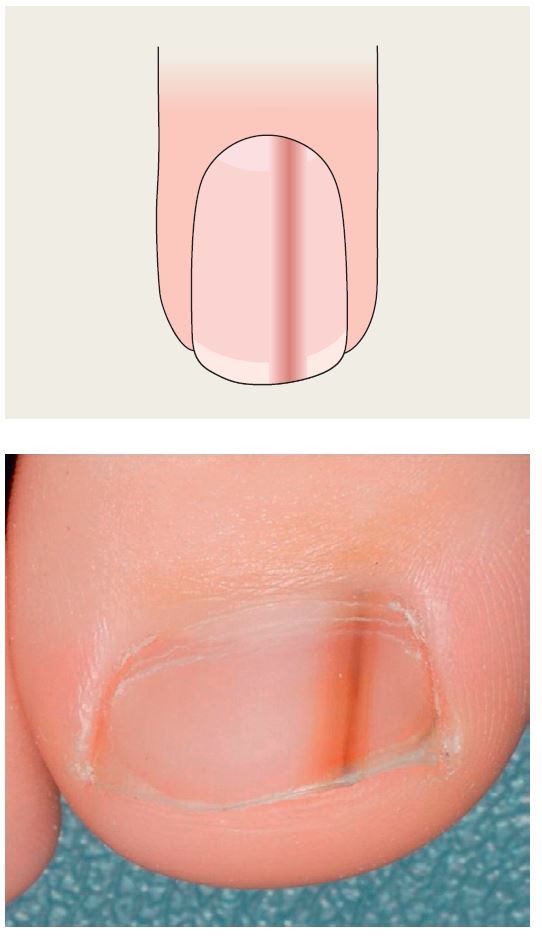
Malalignment
• Most commonly 1st toe(s).
• Lateral deviation of nail plate, often bilateral and congenital.
Nail Patella Syndrome
• Hypoplasia of fingernails, greatest on the thumb, least on the fifth digit, triangular lunulae.
• Absent or hypoplastic patella and renal disease.
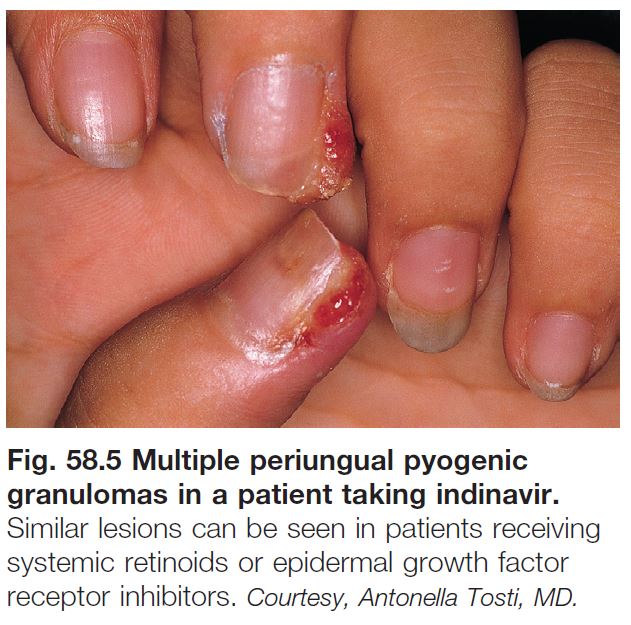
Ingrown Toenails
• Painful inflammation of lateral fold with growth of granulation tissue.
• Can be side effect of drugs.
• Rx: see Table 58.1.
Onychomycosis
• See Chapter 64.
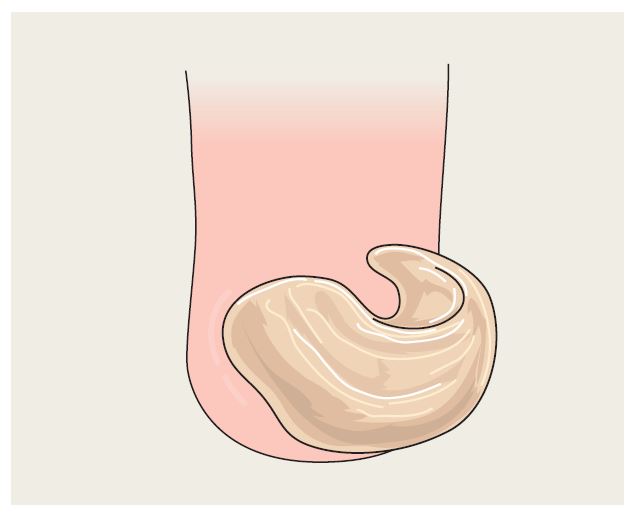
Onychogryphosis
• Most commonly nail(s) of 1st toe(s).
• Curling of nail plate leads to ram’s horn appearance.
• Affects elderly patients.
Subungual Exostosis
• Associated with onycholysis and tender subungual nodule
• Diagnosis confirmed by x-ray
Yellow Nail Syndrome
• Yellow coloration of all or most fingernails > toenails.
• Loss of cuticle, onychomadesis, overcurvature of nail plate.
• Associated with lymphedema and bronchopulmonary disease.
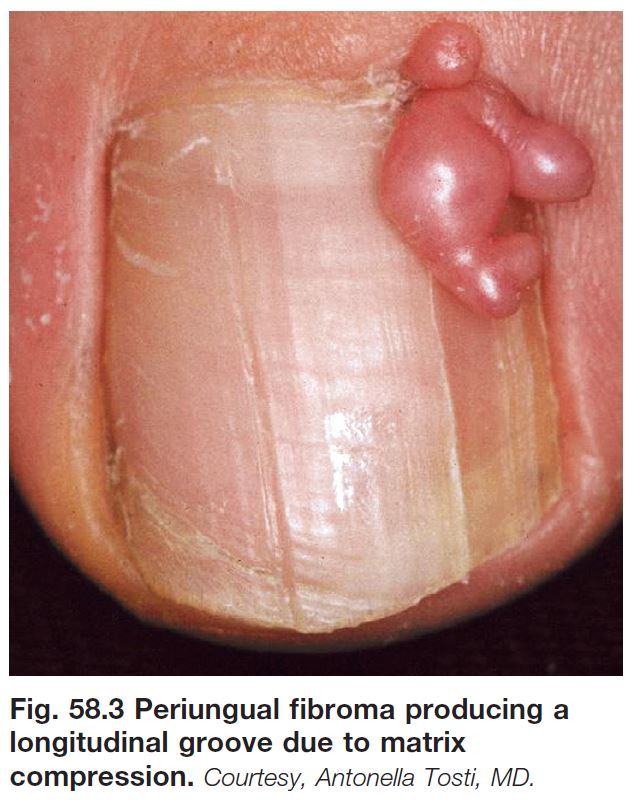
Tumors
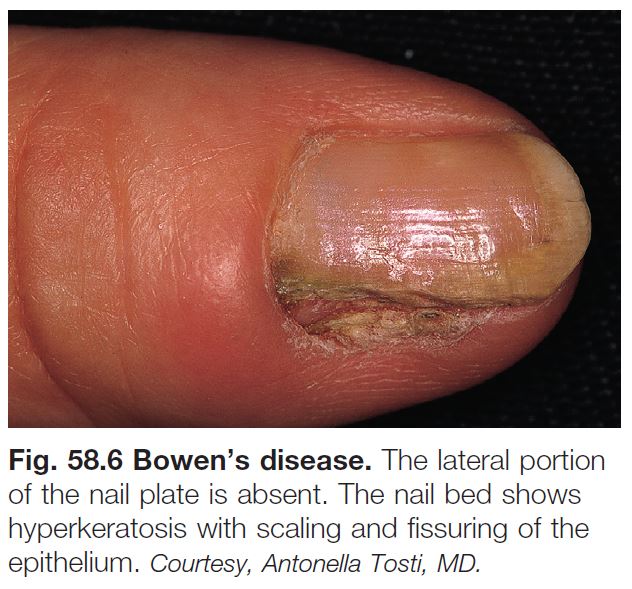
• Various cysts, hyperplasias, and tumors may be seen on the distal digits, including fibromas (Fig. 58.3), myxoid cysts (Fig. 58.4), pyogenic granuloma (Fig. 58.5), glomus tumor (associated with paroxysmal pain) (see Chapter 94), Bowen’s disease (Fig. 58.6), keratoacanthoma (symptoms include pain, rapid growth), melanoma (signs include longitudinal melanonychia [Fig. 58.7], Hutchinson’s sign = pigmentation of proximal cuticle).
Additional details: onycholysis due to psoriasis; onychomadesis after an episode of acute paronychia; apparent leukonychia represents Muehrcke’s lines; multiple Beau’s lines were due to repeated cycles of systemic chemotherapy; proximal nail fold telangiectasias and ragged cuticles due to dermatomyositis.
Additional courtesies: Antonella Tosti, Julie V Schaffer, and Jean L Bolognia.