Key Points
• Irritant contact dermatitis (ICD).
– Accounts for 80% of all causes of contact dermatitis.
– Secondary to a local toxic effect caused by a topical substance or physical insult.
• Allergic contact dermatitis (ACD).
– Accounts for 20% of all causes of contact dermatitis.
– A delayed-type hypersensitivity reaction to a substance to which the individual has been previously sensitized.
– Compared to ICD, more commonly presents with pruritus during the acute phase.
• One of the most common occupational dermatoses is ICD.
• Plants can cause a variety of skin reactions, the most common in North America being ACD to poison ivy.
Irritant Contact Dermatitis
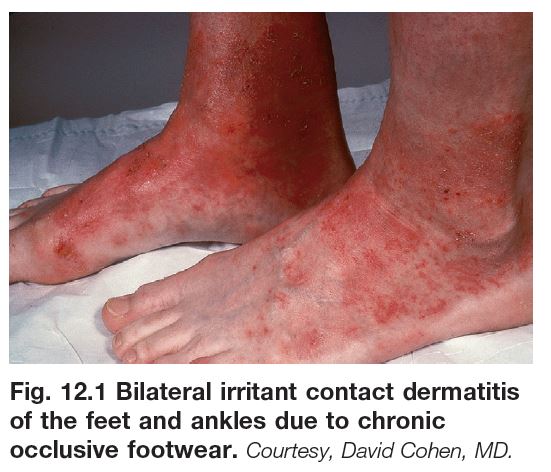
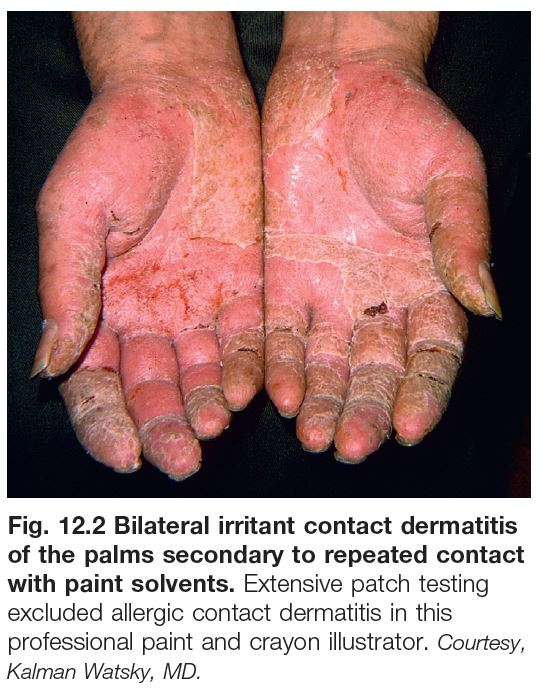
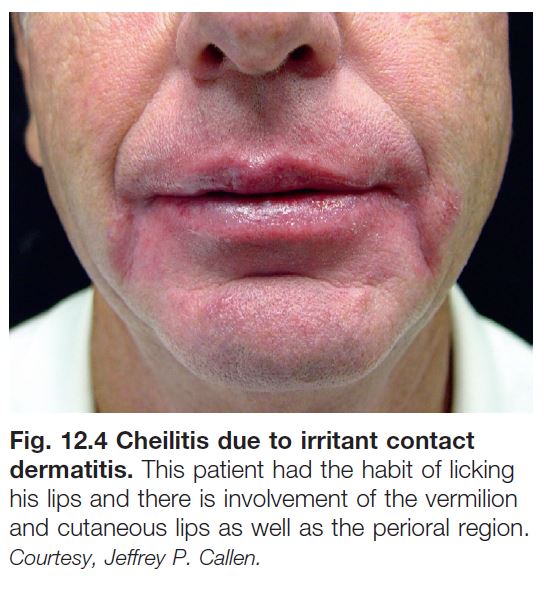
• Localized, non-immunologically mediated cutaneous inflammatory reaction (Figs. 12.1–12.4).
• Secondary to a direct toxic effect.
– Chronic – erythema, lichenification, fissures, and scale.
– Acute – erythema, edema, and vesiculation followed by erosions and scaling; in severe cases may lead to epidermal necrosis (a ‘chemical burn’).
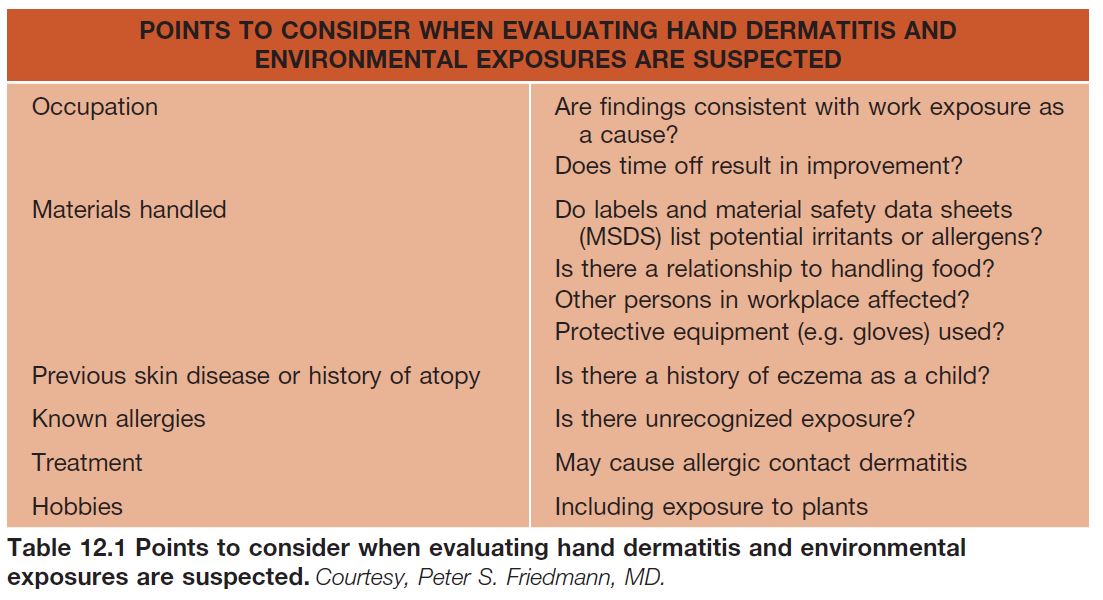
• Commonly affects the hands (see Fig. 13.1); Table 12.1 reviews pertinent questions for when environmental exposures are suspected.
• A common cause of cheilitis (lip-licking; see Fig. 13.4).
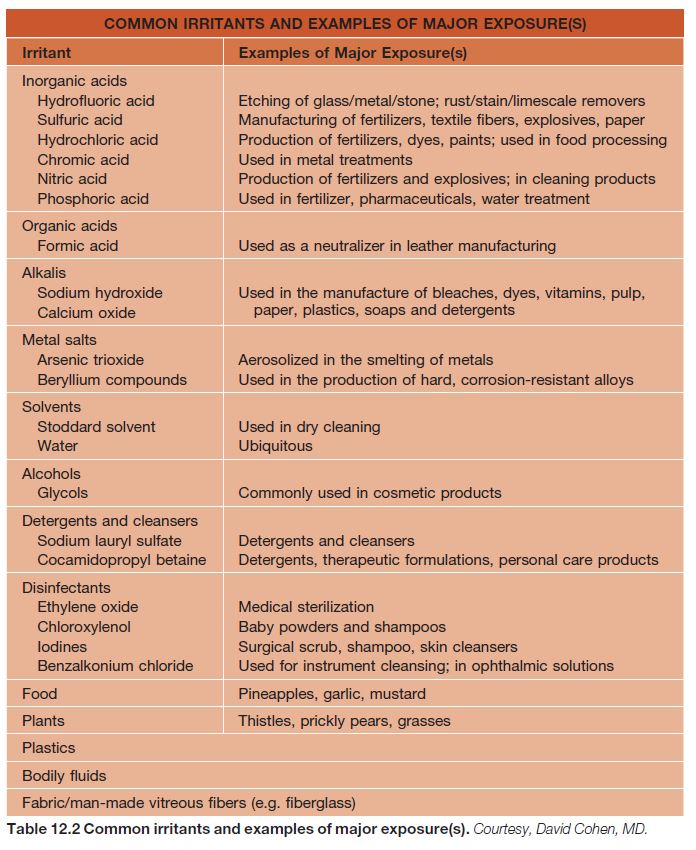
• May be secondary to an occupational exposure (Table 12.2).
– Common causes are soaps and wet work, and less often petroleum products, cutting oils, and coolants.
• DDx: when severe, thermal burn; ACD and other dermatitides; there may be a combination of causes, e.g. ICD and ACD, ICD and atopic dermatitis.
• Rx: primarily avoidance of the irritant.
Allergic Contact Dermatitis
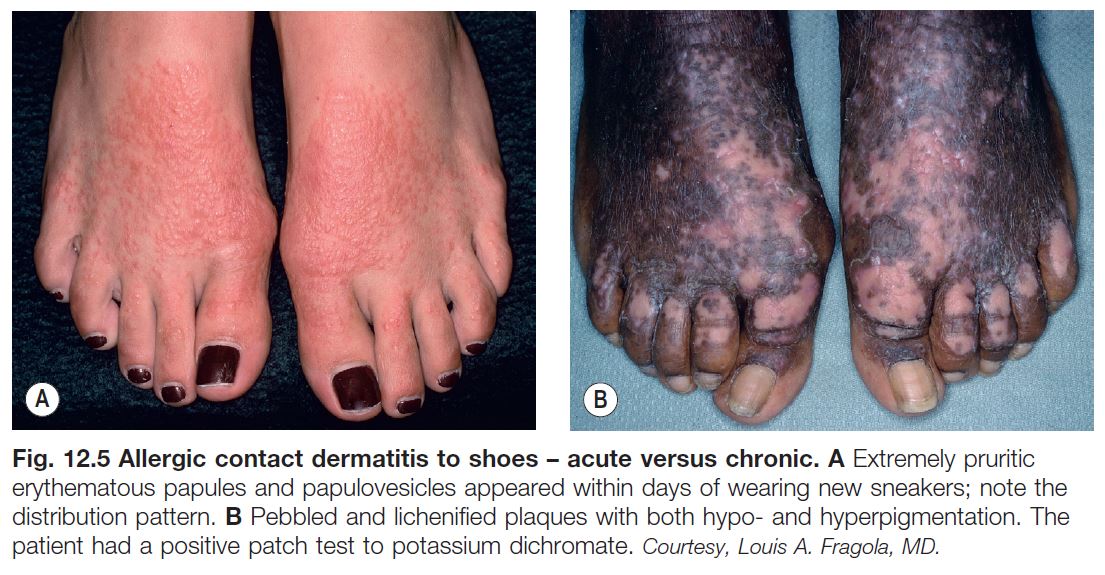
• In contrast to ICD, more commonly presents with pruritus during the acute phase; the chronic phase has significant overlap with ICD (Fig. 12.5).
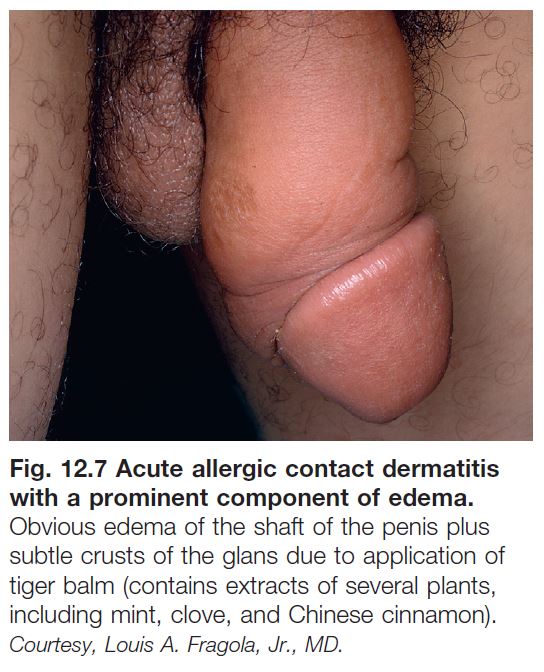
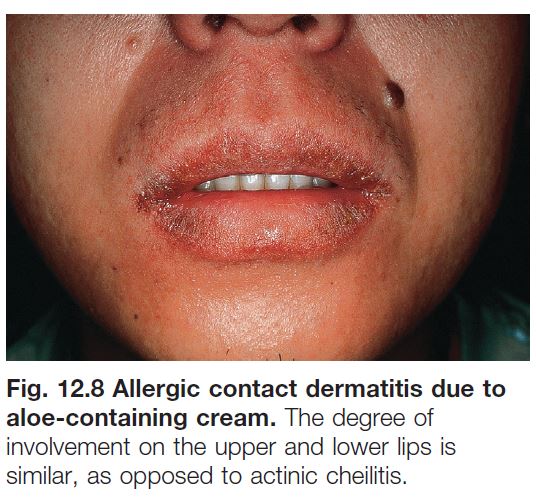
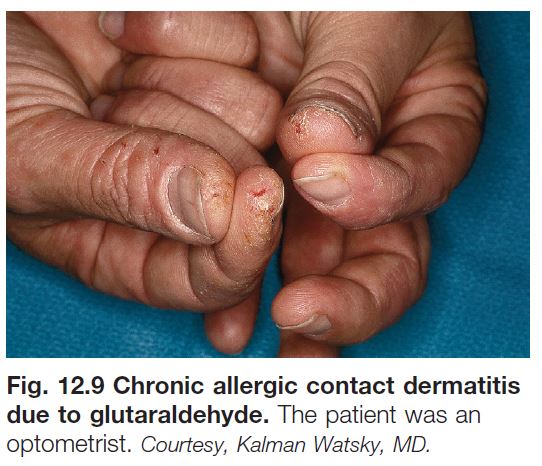
• Initially, well demarcated and localized to site of contact with the allergen (Figs. 12.5–12.10).
– Acute – in addition to erythema and edema, vesicobullae and weeping may develop (Fig. 12.7).
– Chronic – often lichenified with scale (Figs. 12.5B and 12.9).
• Can have autosensitization with extension beyond original site (see Chapter 11).
• Occasionally, there is a diffuse, patchy distribution, depending on the allergen (e.g. body wash or shampoo) and/or concomitant atopic dermatitis.
• Common allergens are metals, fragrances, preservatives, and topical antibiotics, as well as plants, in particular poison ivy/oak (see below) (Fig. 12.10).
• Common causes of occupational ACD are rubber, nickel, epoxy resin, and aromatic amines.
• Suspected allergens should be avoided; an open use test can be tried first but patch testing is required for accurate diagnosis; detailed lists of allergen-containing products are available.
• In patch testing, specific concentrations of allergens are dissolved in petrolatum or water and placed in wells that are then applied to the patient’s back for 48 hours (Figs. 12.11 and 12.12); grading of reactions
is performed at two time points (Table 12.3).
• DDx: other forms of dermatitis (ICD, atopic dermatitis, stasis dermatitis, seborrheic dermatitis), erythematotelangiectatic rosacea, dermatophyte infection.
• Rx: short term: topical and systemic CS depending on severity; long term: avoidance of allergen(s).
Common Allergens
Metals
• Cross-reactivity not uncommon within each broad category.
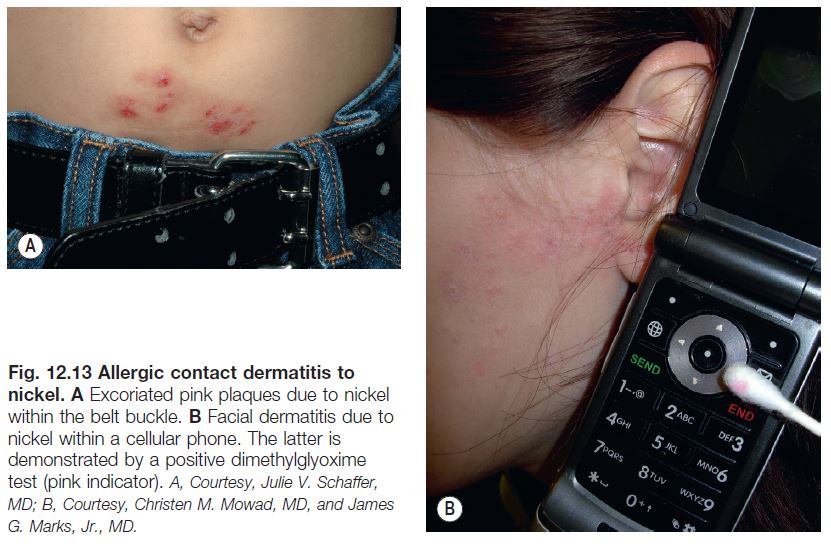
• Nickel – found in costume jewelry, snaps on jeans, backs of watches, belt buckles; dimethylglyoxime test (Fig. 12.13) identifies objects that release nickel (can purchase dimethylglyoxime at http://www.drrecommended.com).
• Chromate – found in metals, leather, cement.
• Cobalt – used to harden metals; cosmetics, enamel, ceramics, hair dyes, and joint replacements.
• Gold – found in jewelry, dental fillings, and some electronics.
Topical Antibiotics
• Neomycin sulfate – found in many overthe- counter preparations (e.g. hemorrhoid creams).
• Bacitracin – in many products, including some that are labeled ‘unscented’.
Fragrances
• Balsam of Peru (Myroxylon pereirae) – one of the naturally occurring fragrances; also found in spices (cloves, Jamaican pepper, cinnamon).
Preservatives
• Formaldehyde – cosmetics and textiles (permanent press), medications, paints.
• Thimerosal – found as a preservative in vaccines, contact lens solution, antiseptics, and cosmetics.
• Quaternium-15 – formaldehyde-releasing preservative; found in shampoos, moisturizers, cosmetics, and soaps.
Other Important Allergens
Topical Corticosteroids
• Can cause ACD in up to 6% of patients.
• Consider CS allergy if an existing dermatitis worsens with CS use or fails to clear; testing with topical tixocortal pivalate (class A) and budesonide (class B) will detect ~90% of CS allergy.
• If CS allergy is suspected/confirmed, use of a CS from a different class can be considered (see Appendix).
Additional allergens include paraphenylenediamine in temporary tattoos and hair dyes, acrylates in artificial nails, thiuram in rubber and makeup applicators, formaldehyde resin in nail polish, components of adhesives, and blue dyes in textiles.
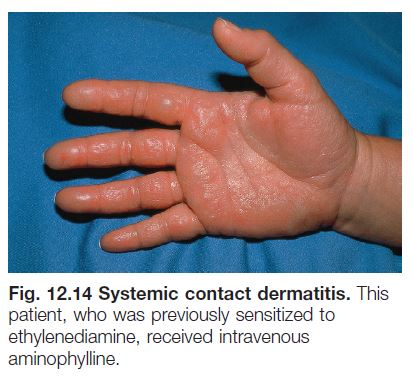
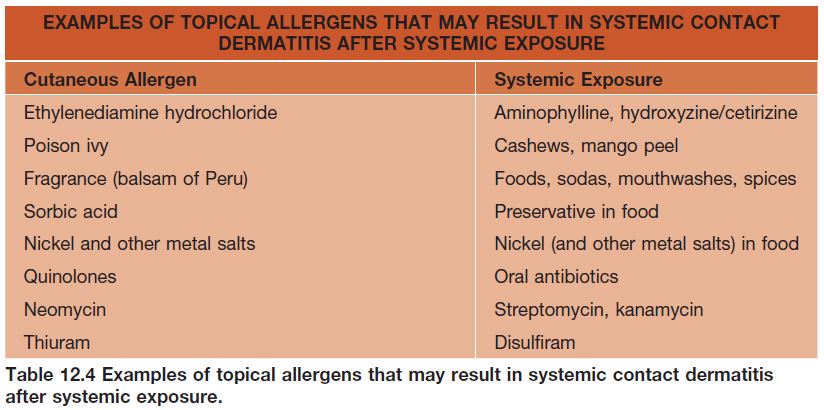
Systemic Contact Dermatitis
• Systemic exposure to a chemical/allergen to which the patient has had prior sensitization (Table 12.4; Fig. 12.14); e.g. administration of oral diphenhydramine to a patient previously sensitized to the topical formulation.
Occupational Dermatoses
• Most commonly an irritant > allergic contact dermatitis.
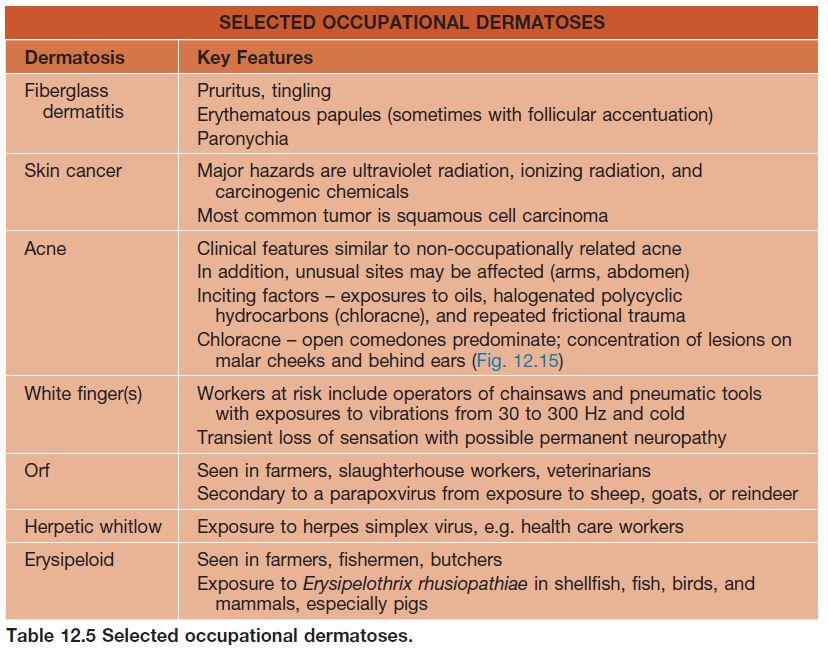
• Other occupational dermatoses include contact urticaria (see Chapter 14), skin cancer, folliculitis (see Chapter 31), contact leukoderma (see Chapter 54), foreign body reactions, and infections (Table 12.5).
Plant Dermatoses
• Plants can cause a variety of skin reactions, including ACD (Fig. 12.10), ICD, urticaria, and phytophotodermatitis (Table 12.6).
• ACD to plants that contain urushiol.
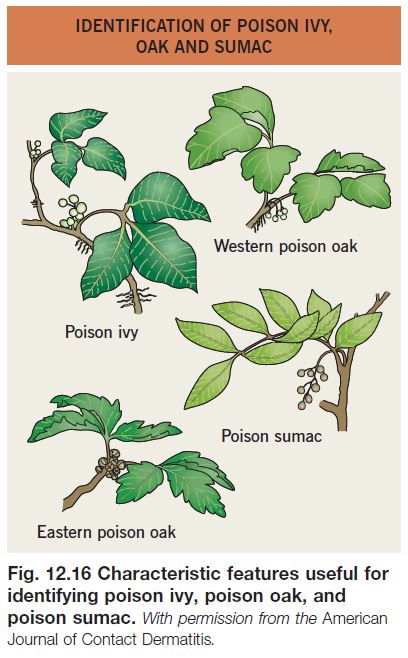
– Commonly secondary to poison ivy, genus Toxicodendron (Fig. 12.16) – compound leaves with three leaflets and flowers/fruits arising from the axillary position; black dots of urushiol often present on leaves.
– Chemicals that cross-react with urushiol are found in the cashew nut tree (nutshell oil and bark), mango tree (leaves, bark, stems, fruit skin), Brazilian pepper tree (sap and crushed berries), Japanese lacquer tree (bark sap), Indian marking tree nut (black juice), and Ginkgo tree (seed coat).
– Allergen-containing smoke can cause respiratory tract inflammation, systemic contact dermatitis, and temporary blindness.
– After contact with urushiol, a sensitized person develops erythema, vesicles/ bullae, and edema within 2 days; the reaction can last 2 or 3 weeks (Fig. 12.10).
– Rx: topical, or if severe, systemic CS; treatment should be for at least 2 weeks, otherwise rebound phenomenon common (i.e., avoid the use of a 6-day Medrol® dose pack).
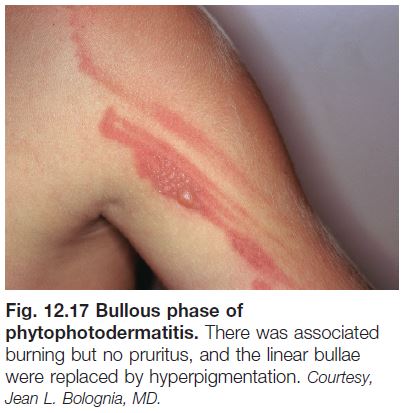
• Phytophotodermatitis.
– Non-immunologic reaction to topical contact with a photosensitizer and subsequent exposure to ultraviolet A light.
– Erythema, vesicles/bullae, and subsequent hyperpigmentation; often in linear streaks or bizarre configurations; however, hyperpigmentation may be the only clinical finding (Figs. 12.17 and 12.18).
– Commonly secondary to furocoumarins (psoralens and angelicins) in plants, e.g. limes, celery, false Bishop’s weed, and rue (Fig. 12.18).