Neural/Neuroendocrine
Neurofibroma
• Skin-colored to pink, soft papulonodule, often on the trunk (see Fig. 50.2).
• Compressible (the tumor often herniates inward upon palpation – this is referred to as the ‘button-hole’ sign); it is sometimes pedunculated.
• Usually solitary in most individuals.
• When multiple, need to distinguish linear form (segmental; mosaic) from a generalized distribution pattern (neurofibromatosis type I) (see Chapter 50).
• Histopathology: wavy, delicate spindle cells with tapered nuclei in a pink stroma.
• Plexiform type has been likened to a ‘bag of worms’ (Fig. 95.1); it is generally on the trunk and proximal extremities, highly associated with neurofibromatosis type I, and prone to malignant degeneration (2–13%).
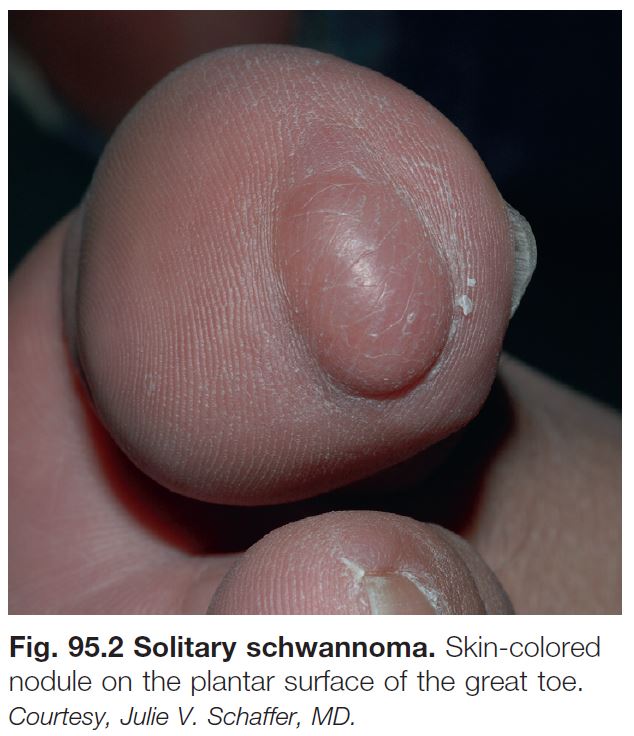
Schwannoma/Neurilemmoma
• Solitary, pink-yellow, soft, smooth papulonodule; generally seen in adults.
• Often on the extremities or head (Fig. 95.2).
• Asymptomatic (rarely painful).
• Histopathology: encapsulated tumor with foci of wavy, spindled nuclei in palisades and foci of myxoid change.
Granular Cell Tumor
• Often in adults; skin-colored to brown-red, firm papulonodule; sometimes ulcerated or verrucous.
• 30% on the tongue.
• Multiple tumors in 10% of patients.
• Histopathology: polygonal cells with oval nuclei and characteristic granular cytoplasm.
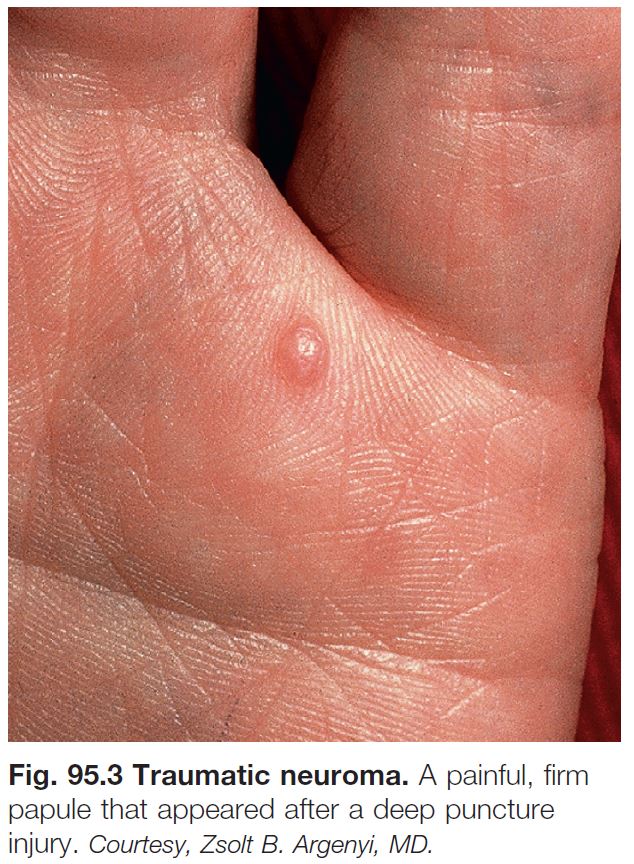
Traumatic Neuroma
• Skin-colored papulonodule(s) at a site of prior trauma.
• Often painful or ‘sensitive’ (Fig. 95.3).
• Histopathology: haphazardly distributed fascicles of spindle cells with tapered nuclei.
Merkel Cell Carcinoma
• In older adults; solitary, rapidly growing, pink to red to violaceous nodule (Fig. 95.4).
• Commonly on the head and neck.
• Aggressive behavior: distant metastases in 40%; 70% survival at 5 years if primary lesion is <2 cm in diameter; 18% survival at 5 years if distant metastatic disease.
• Histopathology: islands or trabeculae of blue cells that on high-power magnification have chromatin that appears speckled like ‘salt and pepper’; characteristically cytokeratin 20 (CK20)-positive and thyroid transcription factor-1 (TTF1)-negative.
• Rx: optimally includes wide excision, accompanied by sentinel lymph node biopsy (SLNB); adjuvant radiation treatment recommended for most patients (exceptions: primary ≤1 cm, SLNB negative, no immunosuppression).
Fibrous/Fibrohistiocytic
Skin Tag (Acrochordon, Fibroepithelial Polyp, Soft Fibroma)
• Common; skin-colored to pink or occasionally hyperpigmented, pedunculated papule.
• Sites of predilection: neck, axilla, groin (Fig. 95.5).
• Can become irritated or infarcted.
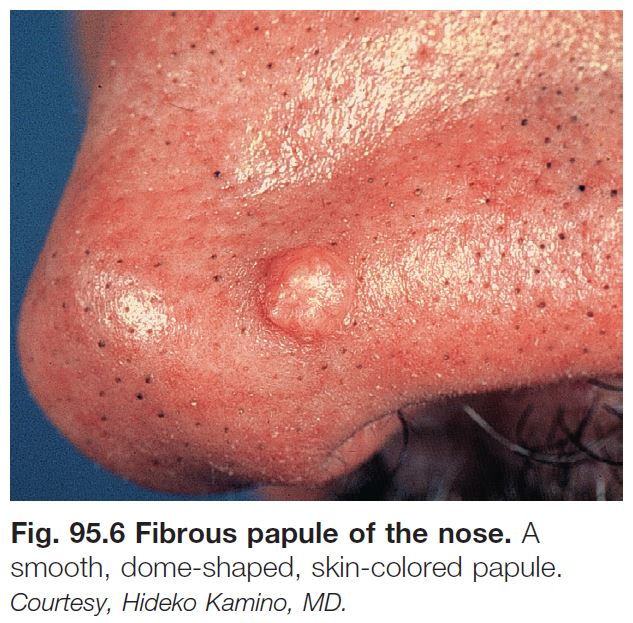
Angiofibroma (Fibrous Papule)
• Solitary, skin-colored to pink, shiny papule; commonly on the nose (Fig. 95.6).
• When multiple, need to consider genodermatoses (e.g. tuberous sclerosis, multiple endocrine neoplasia type I).
• Histopathology: stellate spindle cells in a hyalinized stroma with dilated vessels.
• DDx: basal cell carcinoma, intradermal melanocytic nevus, adnexal tumors.
Pearly Penile Papules
• Multiple, small, white to light pink papules along the corona of the glans penis, often with a multilayered distribution (Fig. 95.7).
• Rx: reassurance.
Dermatofibroma
• 6- to 10-mm pink (especially in fairskinned individuals), tan, or brown papule (Fig. 95.8); firm; dimples inward with lateral pressure.
• Often on the lower extremities; women > men.
• Common; multiple lesions can be seen in normal individuals but also are associated with lupus erythematosus and immunosuppresion (e.g. HIV infection).
• Histopathology: epidermal hyperplasia (sometimes with basaloid induction that resembles basal cell carcinoma) above a spindle cell proliferation that entraps collagen.
• Dermoscopic features are shown in Fig. 1.13.
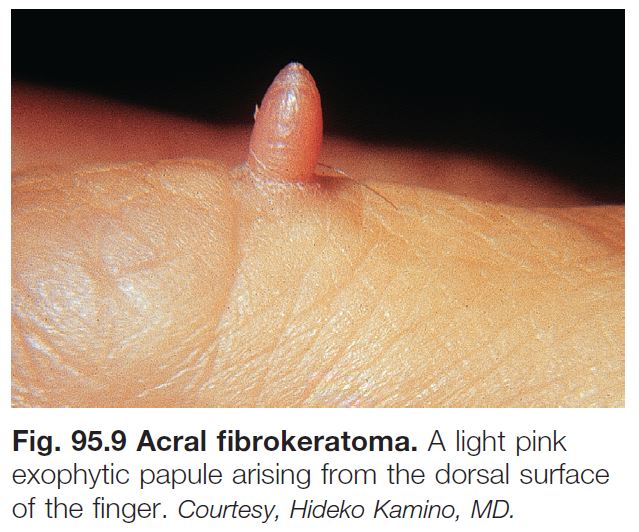
Acral Fibrokeratoma
• 4- to 10-mm solitary, skin-colored to pink, cone-shaped, keratotic papule with a collarette of elevated skin (Fig. 95.9).
• Located on the fingers and sometimes the palms.
Sclerotic Fibroma
• 2- to 9-mm dome-shaped, pearly papule or nodule in adults.
• Slight predilection for the head and neck.
• Can be seen in patients with Cowden disease.
Giant Cell Tumor of Tendon Sheath
• Firm nodule (1–2 cm), generally on the fingers or toes (Fig. 95.10).
• 30% of tumors recur locally.
Nodular Fasciitis
• Benign, reactive process in young adults.
• Rapidly growing subcutaneous nodule (1–5 cm in diameter).
• Commonly on the distal upper extremity.
• Sometimes associated with trauma.
• Histopathology: subcutaneous nodule of elongated spindle cells in a myxoid matrix.
Connective Tissue Nevus
• Skin-colored to yellow-tan (more yellow when composed predominantly of elastic tissue), firm papulonodules or plaques; solitary or multiple (often grouped) (Fig. 95.11).
• Present at birth or arise during childhood.
• May be associated with genodermatoses (e.g. tuberous sclerosis, Buschke–Ollendorf syndrome, Proteus syndrome).
• Histopathology: increased collagen (sometimes subtle) and/or elastic tissue; diagnosis may require special stains for elastic fibers and collagen.
Infantile Digital Fibroma
• Firm, skin-colored to pink papulonodule on the fingers or toes (tends to spare the thumb and great toe) (Fig. 95.12).
• Solitary or multiple; generally present before 1 year of age.
• May recur.
Infantile Myofibromatosis
• One or more skin-colored to pink to violet, firm to rubbery dermal/subcutaneous nodules.
• Most commonly on the head and neck or trunk.
• Rare; lesions present at birth or appear during the first 2 years of life.
• Can have cutaneous lesions alone or systemic involvement (bone, gastrointestinal, kidneys, lungs, heart).
• Tumors tend to self-regress.
• Histopathology: biphasic pattern of spindle cells in nodular arrangements with vessels at the periphery.
Fibromatoses
• Five subtypes, four of which are superficial: (1) palmar (Dupuytren’s contracture); (2) plantar (Ledderhose disease); (3) penile (Peyronie’s); and (4) knuckle pads (Fig. 95.13).
• One deep form: extra-abdominal desmoid tumor.
• Slowly growing nodules or plaques or cord-like tumors.
• Palmar fibromatosis can result in flexion contractures, especially of the 4th and/or 5th finger (see Chapter 81).
• Penile fibromatosis can result in pain and erectile dysfunction.
Muscle/Adipose
Leiomyoma
• Solitary or multiple red-brown papules or nodules, often grouped (Fig. 95.14).
• Sometimes painful.
• Generally on the trunk.
• When multiple, consider association with uterine leiomyomas and papillary renal cell carcinoma (Reed syndrome).
• Histopathology: fascicles of spindle cells with cigar-shaped nuclei that have perinuclear vacuoles.
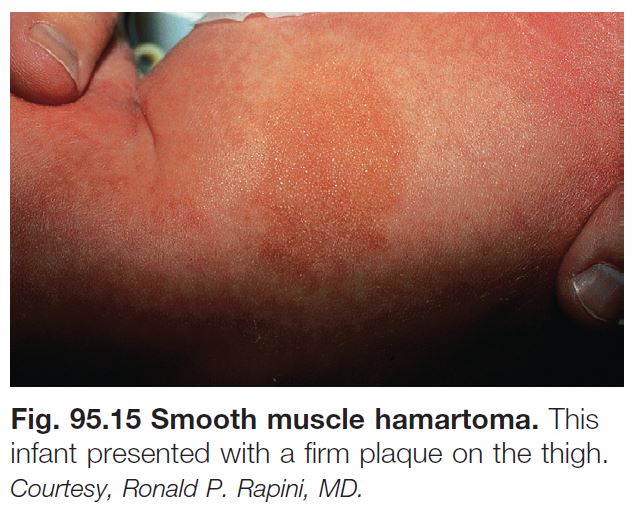
Smooth Muscle Hamartoma
• Congenital or acquired, skin-colored to hyperpigmented plaque on the trunk > proximal extremities (Fig. 95.15).
• Follicular prominence and hypertrichosis may be present.
• May be confused with a congenital melanocytic nevus.
• Is on a clinicopathologic spectrum with Becker’s nevus.
Lipoma
• Common tumor of mature fat; soft, mobile subcutaneous nodule.
• Generally on the trunk and extremities, but any site possible.
• Occasionally painful.
• Multiple lesions may be associated with a lipomatosis (e.g. familial type; Fig. 95.16) or a genodermatosis (e.g. Gardner syndrome, Proteus syndrome).
• DDx: see Fig. 95.17.
Angiolipoma
• Soft, mobile, subcutaneous nodule; often on the forearm in young adults.
• Often painful.
Nevus Lipomatosus
• Grouped, soft, yellow to skin-colored papulonodules on the hips and/or upper thighs(Fig. 95.18).
• Develops during infancy to the first two decades of life.
Soft Tissue Sarcomas (See Table 95.1)
• Rare in comparison to benign soft tissue tumors.
• Generally presents as a nonspecific, deepseated nodule.
• Dermatofibrosarcoma protuberans (DFSP) is characteristically multinodular (Fig. 95.19).
• Most DFSPs have a translocation t(17;22) that fuses the collagen I and platelet-derived growth factor genes; expression of this fusion gene results in high levels of platelet-derived growth factor that stimulates proliferation of fibroblasts.