Achalasia is motility disorder of esophagus. Achalasia is a rare disorder affecting about 1.6 per 100,000 individuals. Both men and women are equally affected. The disease usually occurs between the ages of 25 and 60 years. The primary cause of Achalasia is unknown. Secondary cause of Achalasia can be due to Chagas disease caused by protozoan parasite, Trypanosoma Cruzi which occurs predominantly in Central and South America.
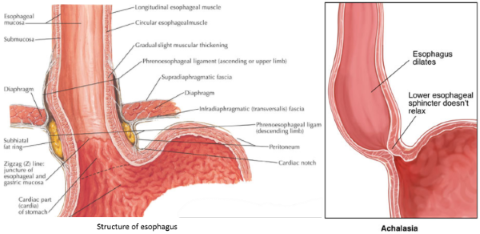
Inflammation and degenerations of nerves in the esophagus causes abnormal propulsion of food when swallowing. Biopsy of esophagus in Achalasia showed decreased number of neurons (ganglion cells) in the myenteric plexuses, and the ganglion cells that are often surrounded by lymphocytes. The inhibitory neurons that produce nitric oxide to relax smooth muscle of esophagus was affected which result food unable to propulse down the esophagus properly. The loss of inhibitory neurons at the lower esophageal sphincter causes the basal sphincter to rise causing sphincter unable to relax when food passing through.
The progression of Achalsia is usually gradual. Patient usually experience symptoms for years before seeking medical attention. The mean duration of symptoms to diagnosis was 4.7 years. Patients are often initially thought to have gastroesophageal reflux disease before the diagnosis of Achalsia is established.
Clinical features:
- Dysphagia (difficult swallowing)
- Regurgitation of undigested food
- Heartburn unresponsive to a trial of proton pump inhibitor therapy (eg. Somac, Nexium)
Diagnosis:
- Esophageal manometry is required to establish the diagnosis. NB: only specialist can order this test
- Gastroscopy should be performed to rule out any other abnormal condition
Without treatment, patients with Achalasia can develop progressive dilatation of the esophagus. Approximately 10% to 15% of patients who have undergone treatment will develop late or end stage Achalasia and up to 5% of patients will require oesophagectomy.
Treatment:
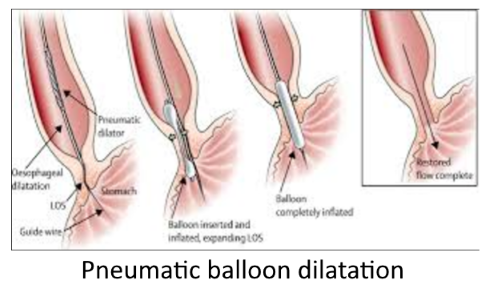
- Pneumatic balloon dilatation of the lower esophageal sphincter which is done under endoscope . Success rate is high about 85% but only lasted for short term
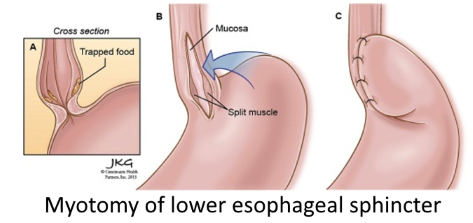
- Surgical myotomy of lower esophageal sphincter by cutting its muscle fibers. This is usually combined with Nissen's fundoplication to prevent reflux. High success rate of 90% but lasted for medium term. There are risks of reflux, perforation of esophagus, pneumothorax, bleeding, vagus nerve injury and infection from the procedure.
- Botox injection. This therapy can be considered in patients who are not a good candidate for pneumatic balloon dilatation or surgical myotomy of lower esophageal sphincter. Botox is injected into the lower esophageal sphincter to paralyse it allowing food or fluid to pass through the esophagus. However, it lasted for short period of time and require retreatment within 6 to 12 months. Repeated Botox injection can also make surgical myotomy of lower esophageal sphincter more difficult if the patient needs it in future.
- Medications such as Nifedipine or Isosorbide dinitrate can used to treat Achalasia but they are not effective.
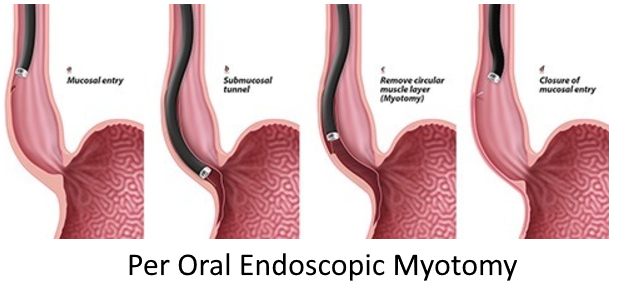
- Per-oral endoscopic myotomy is a procedure where the specialist make a cut in the esophageal mucosa (inner lining), and the endoscope is passed through the cut into the the esophageal submucosa (deeper lining), creating a submucosal tunnel that is extended into the upper stomach part. A diathermy scalpel is then passed through the endoscope to cut the muscle of the muscularis propria (muscle lining) in and around the lower esophageal sphincter. This procedure is often combined with fundoplication to prevent reflux. Complications of this procedures can be pneumothorax, bleeding, muscle perforations and pleural effusions. There is also not much research on this procedure and the long term benefit or adverse effects are yet to be seen.